Constipation 101: A Parent's Guide to Understanding and Managing Kids Constipation
If you've ever felt like you're constantly tracking your child's bowel movements or googling "constipation tips for kids" at 2 AM, you're not alone. Constipation is one of the most common digestive issues in children, affecting millions of kids everywhere. Chronic constipation can lead to pain, stool withholding, or even accidents that leave both you and your child feeling frustrated and stuck.
But here's what most parents don't realize: constipation is rarely just about fiber and water (although it's a great place to start!). If you've already tried the prune pouches, Miralax, + pear juice and nothing's really sticking, there's likely something deeper going on. Let's walk through what constipation really is, why it's more complex than you've been told, and when it's time to look at the whole picture.
Why You Should Be Concerned About Chronic Constipation
When constipation becomes chronic, it can have ripple effects throughout your child's body and daily life:
Toxin buildup: When stool sits in the colon too long, the body can reabsorb waste products that were meant to be eliminated. This can increase discomfort, bloating, appetite suppression, and overall inflammation signals in the gut - all which can absolutely affect mood, energy, and behavior.
Impact on appetite: When kids are backed up, they often feel full and have low appetites. This can worsen picky eating habits and potentially affect growth. It becomes a cycle where constipation impacts eating, and poor eating worsens constipation.
Soiling accidents: These can occur once or multiple times a day due to overflow from a full rectum. The child cannot control these leaks. This is upsetting for everyone. Children feel embarrassed or may be teased, while parents feel frustrated and sometimes angry. Understanding that this is a medical issue, not a behavioral one, is crucial.
Pain creates avoidance: When bowel movements are painful, children can learn to avoid going to the bathroom. This causes more backup, which makes the pain worse, which causes more fear and avoidance. It's a vicious cycle that's hard to break without addressing the root cause.
Could it be encopresis?
Encopresis basically means stool is leaking or being passed involuntarily because the normal sensation and control around bowel movements has been disrupted. This is the part that confuses (and worries) a lot of parents. Your child might be constipated, but you're also finding stool in their underwear multiple times a day. How does that make sense?
Here's what happens: Some children start holding their stool, often because it hurt once, and they're scared it will hurt again. Over time, the muscles stretch and weaken, and the nerves stop signaling that the rectum is full. The rectum stays filled and stretched, creating a reservoir of stool. This withholding can sometimes look like pushing (it's hard to tell the difference), but they're actually holding it in. Over time, the colon can expand and create a pouch-like area where stool collects.
Think of encopresis like a clogged pipe. When there's a hard mass blocking the way, loose or liquid stool can leak around it. The result is small streaks of stool in underwear or diapers throughout the day, followed by one massive, painful bowel movement every few days. Understanding this is the first step toward breaking the cycle.
Photo from Nemours KidsHealth (https://kidshealth.org/en/parents/encopresis.html)
Why Constipation Is More Complex Than You Think
Fiber and water are a great starting point. But for a lot of kids, they’re not enough. If you've already addressed the basics and you're still stuck, it's because there are other factors at play.
Nutrition & Digestion
What your child eats (and doesn’t eat) affects far more than just fiber intake. Your child could be eating all the right things and still not absorbing them properly. Digestion is about more than what goes in - it's about what the body actually does with it. Several key nutrients play a direct role in keeping the digestive system moving:
Inadequate fiber is often the first thing addressed - but the type and amount of fiber matters. Soluble fiber is best for constipation because it forms a gel, which softens stool, supports motility, and feeds beneficial bacteria. Insoluble fiber, on the other hard, may speed transit but cause more pain and discomfort.
B vitamins support the nervous system that controls gut motility (the gut’s ability to move things along). Low B vitamins can quietly slow everything down.
Inadequate calories overall can reduce gut motility. When kids aren’t eating enough, the digestive system can become sluggish.
Low choline (found in eggs, meat, and fish) impairs bile production. Bile isn’t just for fat digestion; it also stimulates the colon. Without enough bile flow, stools can become harder and more difficult to pass. If your child avoids greasy foods or gets belly pain after fatty meals, this could be a clue.
Poor absorption of fat-soluble vitamins (A, D, E, K) can signal that the gut isn’t digesting fat well, which often goes hand in hand with sluggish bile flow and constipation.
Undigested food in stool (yes, this is something we can actually test for) is a sign that the body isn't breaking food down properly. If your child's gut isn't producing enough digestive enzymes, whole proteins from meat or vegetables can pass through undigested, which means they're eating the food, - but not actually getting the nutrition from it. Low pancreatic elastase on a stool test can confirm this.
Motility
Motility refers to the gut’s ability to physically move contents through the digestive tract. Several things can disrupt this:
Fluid and electrolytes are essential and water alone isn’t always enough. Some kids need more sodium or minerals to help the colon retain water in the stool.
Low muscle tone (hypotonia) can affect the muscles of the digestive tract, making it harder to push stool through.
Chronic stress shifts the body into “fight or flight” mode (sympathetic nervous system), which slows digestion. Our gut needs to be in a “rest and digest” (parasympathetic) state to work well.
Dysregulated gut–brain signaling means the communication between the gut and the brain is off. The gut has its own nervous system (sometimes called the “second brain”), and when that signaling is disrupted by stress, trauma, or chronic gut issues, motility suffers.
Microbiome
The trillions of bacteria living in your child’s gut play a huge role in digestion. Here’s what can go wrong:
Dysbiosis (an imbalance in gut bacteria) can slow motility. Some kids naturally have higher levels of methane-producing bacteria, and methane literally slows the movement of stool through the colon. Sulfur-producing bacteria can add more gas, odor, and discomfort too.
Low butyrate production is a big one. Butyrate is a short-chain fatty acid that gut bacteria produce when they ferment fiber. It feeds the cells lining the colon and helps keep things moving. Low butyrate = sluggish colon.
Reduced fermentation of fiber happens when beneficial bacteria are depleted. Without the right bugs to break fiber down, even a fiber-rich diet won’t have the same constipation-relieving effect.
Inflammation
Chronic gut inflammation is another layer that rarely gets explored in standard pediatric visits:
Increased intestinal permeability (often called “leaky gut”) means the gut lining has become more porous than it should be, allowing bacteria, toxins, and undigested food particles to pass through into the bloodstream. This triggers an immune response that drives inflammation throughout the body and GI tract.
Immune activation in the gut can disrupt the delicate environment that healthy digestion depends on, further slowing motility and worsening the constipation cycle.
Standard medical tests won’t show you this. Functional markers like zonulin (a marker of leaky gut) and secretory IgA (which can indicate immune stress in the gut) require comprehensive stool testing to detect.
Potty Training and Behavioral Withholding
Constipation and withholding are incredibly common during and after potty training. Many children experience a painful bowel movement during this transition and develop a fear response, they start holding their stool to avoid the pain happening again. This creates the cycle we discussed earlier with encopresis.
While behavioral interventions (like scheduled potty sits and positive reinforcement) can help, they often aren't enough if the underlying issue is that the stool is still hard and painful. This is where nutrition support becomes critical. When we address the root causes - gut bacteria imbalances, proper hydration and mineral balance, adequate fiber intake, and digestive support - we make it physically easier and less painful for your child to go. That's when the behavioral strategies can actually work.
Picky Eating and Feeding Difficulties
Picky eating and constipation often go hand-in-hand, creating a frustrating cycle that's hard to break. Picky eaters tend to avoid the very foods that support healthy digestion: fruits, vegetables, and protein - while gravitating toward processed, beige carbohydrates like crackers.
These preferred foods are typically low in fiber and require more water to process and move through the digestive tract. When kids aren't eating enough fiber-rich foods AND aren't drinking enough fluids (which is a challenge for most constipated kids), constipation becomes inevitable.
But here's where it gets tricky: when a child is constipated and backed up, they often feel full and have low appetites. This makes them even pickier about food, which worsens the constipation, which worsens the appetite, which makes them pickier. It's a vicious cycle.
This is why a one-size-fits-all approach doesn't work for picky eaters with constipation. You need a personalized strategy that considers your child's sensory preferences, addresses their gut microbiome, and breaks the constipation-picky eating cycle.
Why Functional Testing?
Most of the time, constipation is diagnosed based on your child's symptoms and medical history. You know your child best, and if something feels off, trust that instinct. Your pediatrician may run standard tests or prescribe Miralax and send you on your way.
But here's what often gets missed: standard medical tests won't show you gut bacteria imbalances, inflammatory markers like zonulin (a marker of leaky gut) or secretory IgA (which can indicate food sensitivities), bile flow issues, digestive enzyme insufficiency, or nutrient deficiencies that could be contributing to constipation. Comprehensive functional testing can reveal these underlying issues - things like elevated inflammatory markers in the gut, low pancreatic elastase indicating poor digestion, pathogenic bacteria or parasites that are disrupting normal gut function, and specific bacterial imbalances that slow motility.
That's where functional testing comes in, and where a deeper, more personalized approach makes all the difference. Learn more about our microbiome testing options here.
What Actually Helps
Dietary Strategies
Fiber: Fiber adds bulk to stool and helps it move through the digestive system - but only if your child's gut is functioning well enough to handle it. Too little fiber slows everything down. Too much too quickly can make constipation worse, especially in kids with sensitive tummies or bacterial imbalances. There's a "Goldilocks zone" for fiber that's different for everyone (and it can change with tolerance, too!). A good rule of thumb for kids is age + 5 grams of fiber per day.
Sorbitol: Foods like pears, prunes, plums, and peaches contain sorbitol, a natural sugar alcohol that helps pull water into the colon. Most kids can have 4oz juice per day. Make sure it’s non-diluted - we want the osmotic effect!
Hydration: Water alone isn't always enough. Some kids need more sodium or minerals in their fluids to help the colon retain water in the stool. This is especially true if your child is a poor eater or has been chronically constipated for a long time. A pinch of salt in water, coconut water, diluted juice, or mineral drops can help.
Healthy Fats: Adequate dietary fat supports bile release and stool lubrication, which can improve stool consistency and ease of passage. Medium-chain triglycerides (MCTs) may be beneficial when fat digestion or bile flow is limited.
Magnesium: Magnesium is a mineral that draws water into the intestines and relaxes the muscles of the digestive tract, which can help soften stool and promote bowel movements. However, there are different forms of magnesium (citrate, glycinate, oxide), and they work differently in the body. The form and dosage need to be individualized. Too little won't help, and too much can cause loose stools or stomach upset.
Foods that support digestion: Some foods naturally support digestion from a motility and bile flow perspective: warm lemon water, bitter foods (like arugula), chia seeds, kiwi, and magnesium-rich foods.
Probiotics: Probiotics support gut bacteria balance and can be helpful for constipation, but not all probiotics are created equal. Many parents grab whatever is on the shelf at the pharmacy without realizing that the specific strains and potency matter significantly. For kids, I typically look for a high-quality probiotic with at least 5 billion CFU (colony-forming units) and 10+ different types of bacteria. But here's the catch: the specific strains your child needs depend on their individual gut microbiome, which is why comprehensive stool testing is so valuable. Without testing, you're essentially guessing and hoping you picked the right one.
Constipation Smoothie for Kids: One strategy that works well for many families is incorporating a constipation-relief smoothie. Smoothies can pack fiber, hydration, probiotics, and nutrients into one kid-friendly package.
Kids Constipation Smoothie Recipe
Ingredients:
1 cup frozen blueberries
1/2 cup frozen cauliflower (your child won't taste it, promise)
1/2 ripe banana (ripe is important…think banana bread ripe)
1 tablespoon ground flaxseed or chia seeds
1/2 cup yogurt
1/2 cup coconut water
1/4 cup prune juice
1 teaspoon MCT oil (optional, but helpful for gut motility)
Optional: 1/2 teaspoon vanilla extract and a drizzle of honey
Instructions: Blend all ingredients until smooth. Add more liquid if needed to reach your child's preferred consistency. The blueberries give it a fun blue color, the fiber and sorbitol help soften stool, the probiotics support gut health, and the MCT oil can help stimulate bowel movements.
This smoothie combines multiple constipation-fighting strategies in one glass, but how often to serve it and whether to adjust the ingredients depends on your child's individual digestive function and tolerance.
Supportive Interventions
Movement: Physical activity stimulates digestion and helps keep the bowels moving. Anything that twists, bends, or bounces can encourage peristalsis. Even a few minutes of playful movement before sitting on the toilet can help.
Toilet Routine and Positioning: Have your child sit on the toilet for 5-10 minutes after meals, when the body's natural gastrocolic reflex helps trigger bowel movements. Keep it light and stress-free. For older or taller kids, use a step stool so their feet are supported and their knees are above hip level. This position helps relax the anal sphincter and makes it easier to pass stool.
Epsom Salt Baths: Warm water relaxes muscles, and Epsom salt is magnesium sulfate (a magnesium salt) meaning your child may absorb a little extra magnesium right through the skin. Athletes often soak in epsom salt baths to soothe sore muscles, and the colon is a muscle, too!
Gentle Massage: A light abdominal massage (firm but gentle pressure just under the ribcage, working clockwise) can help the digestive tract do its job.
Photo from Mindful Nutrition (https://mindfulfamilymedicine.com/the-i-love-you-ilu-digestive-massage/)
Medications: Sometimes stool softeners or laxatives are necessary. But these should always be used as part of a larger plan, and not as a Band-Aid that masks deeper issues.
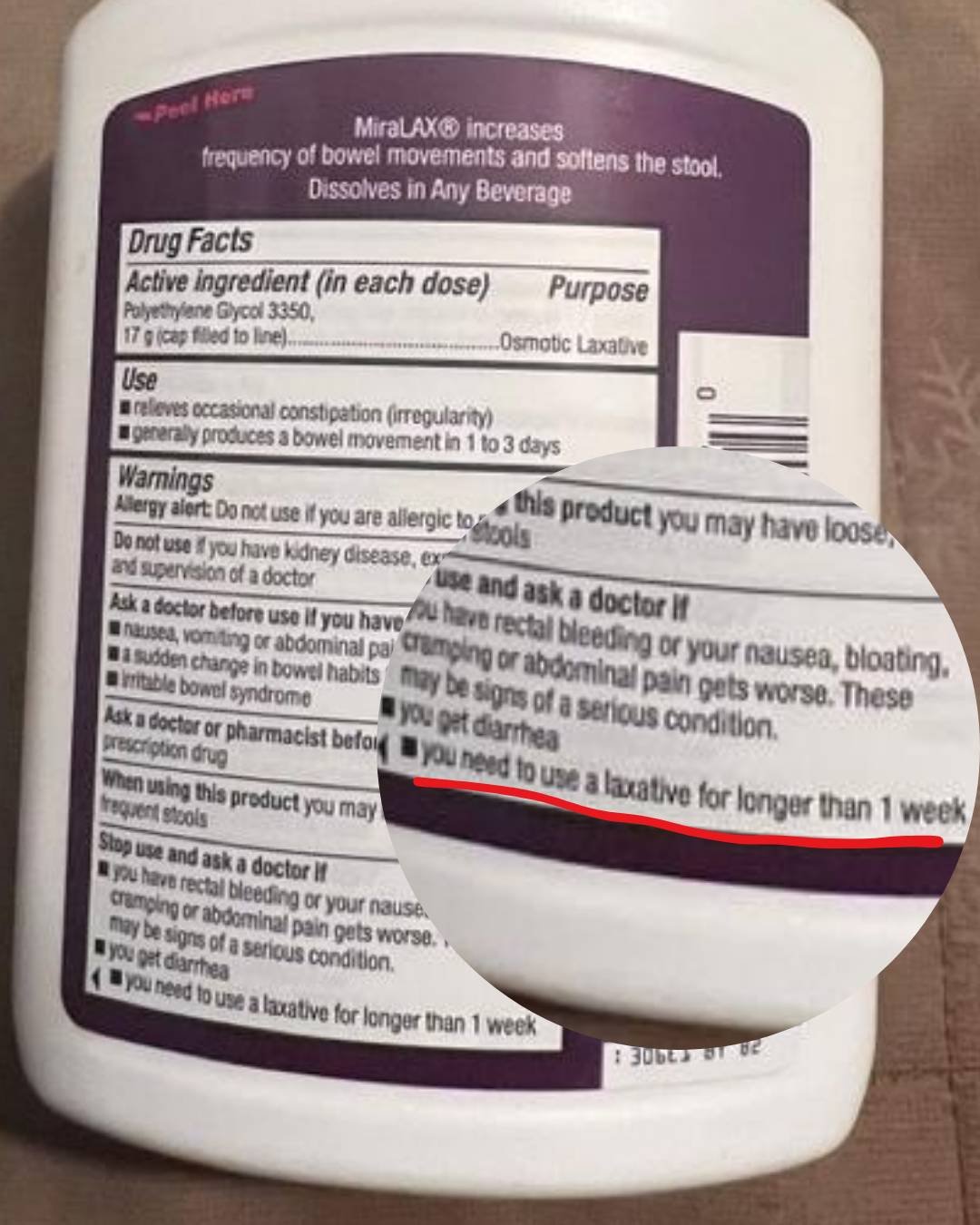
Here's something most parents don't realize: Miralax's label instructions recommend discontinuing use after 7 days. Yet pediatricians routinely prescribe it for months - even years - without looking deeper at what's actually causing the constipation. If your child has been on Miralax for an extended period and you're still struggling, that's a clear sign something else needs to be addressed.
The Bottom Line
If you've been trying the standard recommendations: more fiber, more water, prune juice, Miralax - and you're still stuck in the cycle of constipation, soiling accidents, or picky eating that won't budge, it's because there's something deeper going on. Constipation is rarely just one thing. It's often a combination of gut bacteria imbalances, bile flow issues, nervous system dysregulation, nutrient deficiencies, and learned withholding behaviors.
The truth is, you can't Google or Instagram your way out of a complex digestive issue. What your child needs is a personalized plan that addresses their specific imbalances, not a one-size-fits-all protocol. That's where comprehensive testing and individualized nutrition support make all the difference.
If constipation is affecting your child's comfort, confidence, or quality of life, don't settle for "they'll grow out of it." You don't have to keep playing detective with their poop, appetite, and food variety.
A pediatric dietitian who understands complex feeding and digestive challenges can help you get to the root cause, create a clear roadmap, and finally break the cycle. When root causes are addressed, many families see improvement within 2-4 weeks of implementing a personalized protocol based on testing results.
Ready to stop guessing and start getting real answers? Schedule a free 15-minute consultation to discuss whether comprehensive stool testing is right for your child!
References:
Tabbers MM, DiLorenzo C, Berger MY, et al. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014;58:258–74.
Hyams JS, Di Lorenzo C, Saps M, et al. Functional Disorders: Children and Adolescents. Gastroenterology. 2016.
Benninga MA, Faure C, Hyman PE, et al. Childhood Functional Gastrointestinal Disorders: Neonate/Toddler. Gastroenterology. 2016.
Gordon M, de Geus A, Banasiuk M, et al. ESPGHAN and NASPGHAN 2024 protocol for paediatric functional constipation treatment guidelines. BMJ Paediatr Open. 2025;9(1):e003161.
Bashir S, Faye AS. Pediatric Functional Constipation: A New Challenge. Advanced Gut & Microbiome Research. 2024.